Inflammation of the Aorta
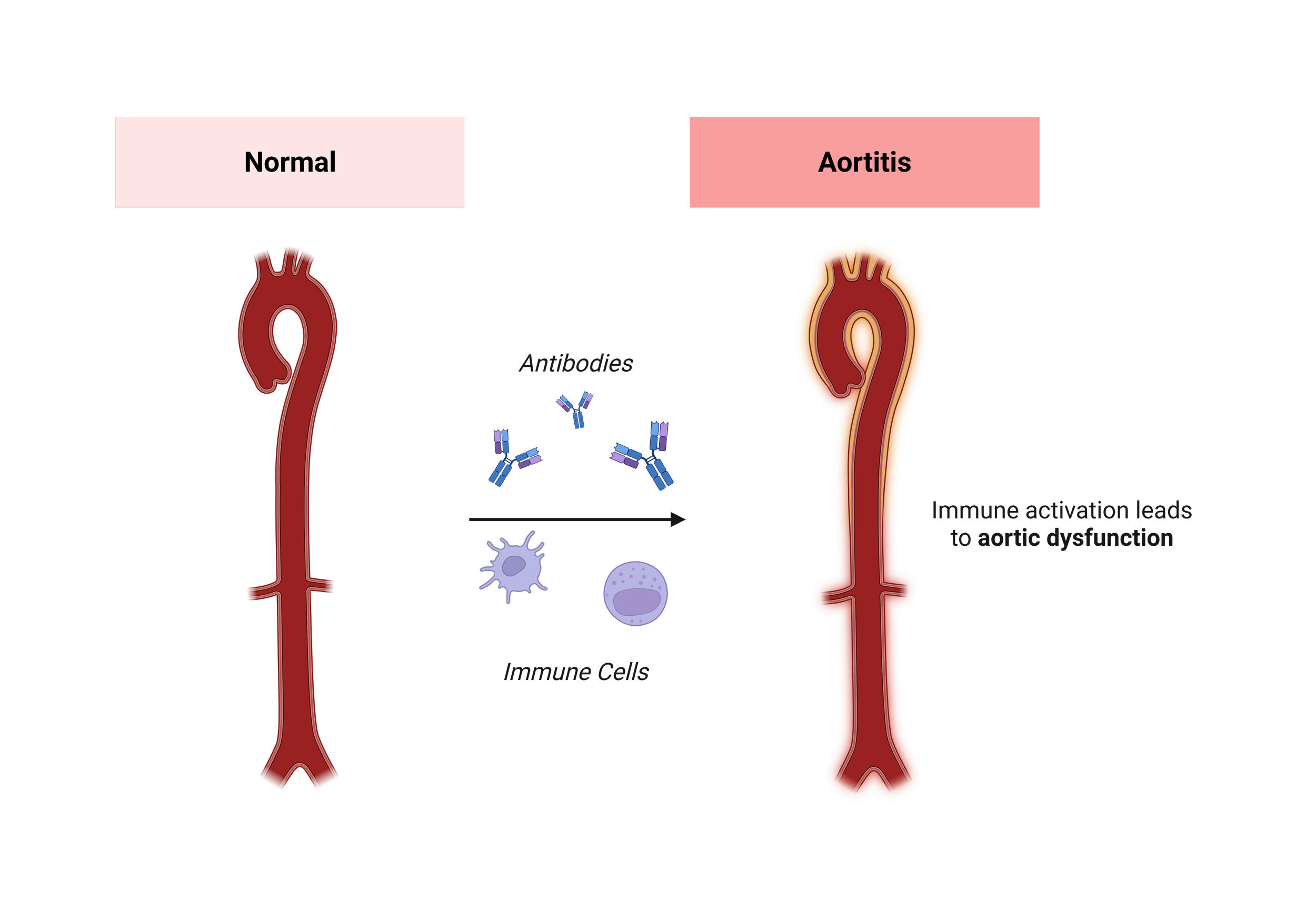
What Is Inflammation of the Aorta?
Inflammatory aortic disease happens when the wall of the aorta becomes inflamed. This is different from wear-and-tear changes, because it is driven by the body’s own immune system or by infections. When inflammation attacks the wall, it can weaken it, change its structure, and make it prone to serious complications.
Although rare, inflammation of the aorta is important because it can lead to aneurysms, narrowing, or even dangerous problems like aortic dissection.
Why Does It Happen?
Inflammation in the aorta can have different causes:
Autoimmune diseases
In these conditions, the body’s immune system mistakenly attacks its own tissues. When it targets the aorta, the media is especially at risk because it contains the elastic fibers that give the aorta its strength.
Giant Cell Arteritis: usually affects older adults and can cause headaches, vision problems, and inflammation in the branches of the aorta.
Takayasu Arteritis: often develops in younger people, more commonly women, and can cause narrowing or blockage of large vessels like the aorta and its branches.
Other autoimmune diseases: Conditions such as lupus or rheumatoid arthritis can sometimes inflame the aorta as part of a broader illness.
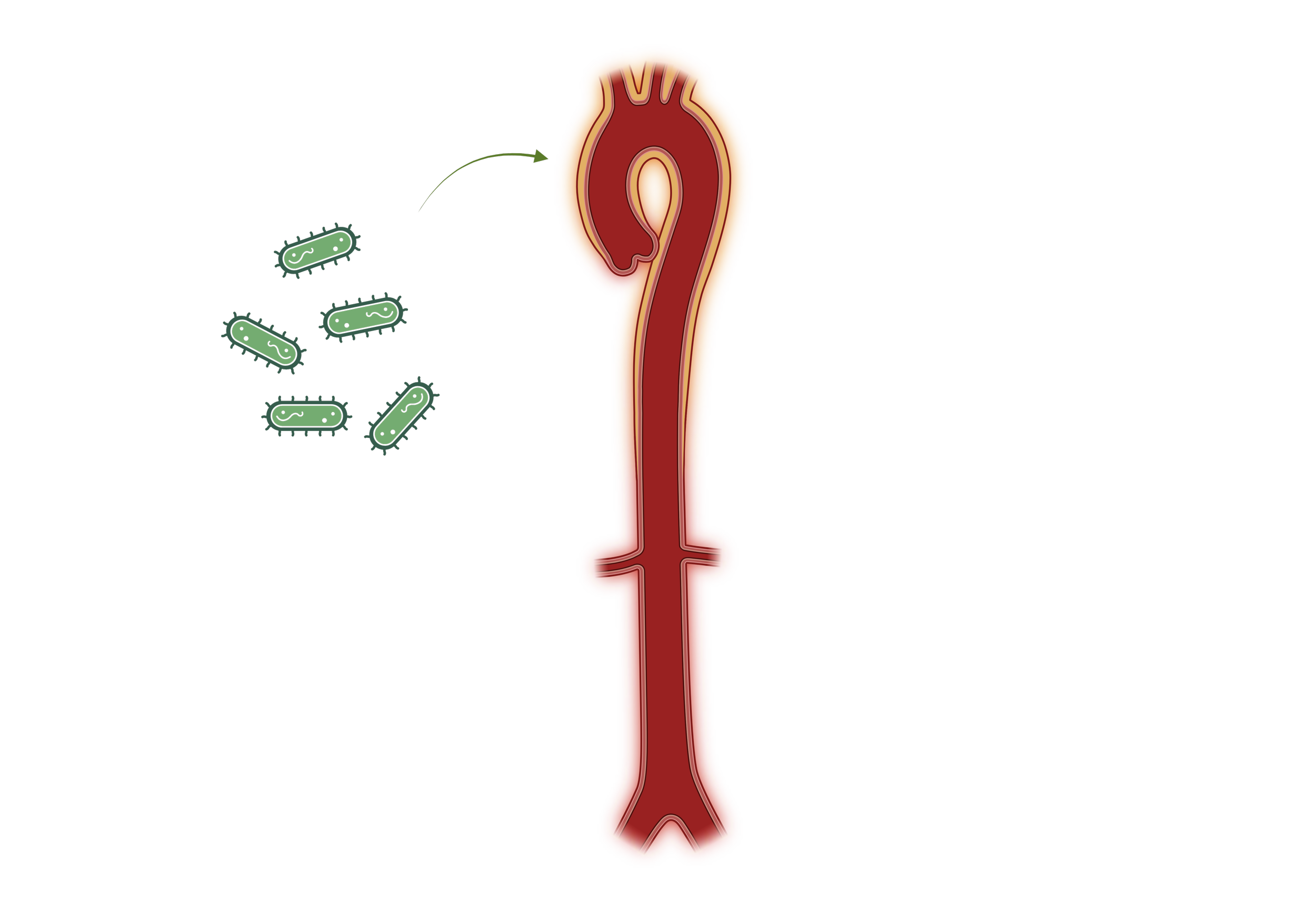
Infections
Although rare in modern medicine, infections can directly affect the wall of the aorta. This is sometimes called infectious aortitis.
Bacterial infections: Certain bacteria can reach the aorta through the bloodstream, usually in people with weakened immune systems or preexisting aortic disease.
Syphilis: Before antibiotics, syphilis was a major cause of aortic inflammation, leading to aneurysms. Today it is seen much less often but remains a historic example.
Tuberculosis: In rare cases, this infection can spread to the aorta and weaken its wall.
Other inflammatory causes (Immune-mediated):
Sometimes the aorta becomes inflamed due to conditions not strictly classified as autoimmune or infectious.
IgG4-related disease: a disorder where the body produces excess immune proteins (IgG4) that can inflame and thicken the wall of the aorta and other organs.
Vasculitis of other origins: inflammation of blood vessels (vasculitis) can occasionally extend into the aorta, damaging mainly the media and adventitia, and making the vessel vulnerable.
In each case, the result is changes in the wall’s structure that make it weaker or stiffer.
How Does It Show Itself?
Symptoms can be quite general at first, which sometimes makes recognition difficult. Patients may notice:
Ongoing fever, fatigue, or unexplained weight loss
Pain in the chest, back, or abdomen if the wall becomes damaged
Arm or leg weakness due to reduced blood flow when inflamed areas narrow blood vessels
Headache, jaw pain, or vision problems in conditions like Giant Cell Arteritis, when multiple large arteries are involved
Often these symptoms are combined with laboratory signs of inflammation that doctors can measure.
Possible Complications
If inflammation of the aorta is not detected and treated, the following problems can develop:
Aneurysms: weakening of the media can cause the wall to bulge outward.
Aortic dissection: inflammation-related weakening makes the wall prone to tears in the intima, allowing blood to enter the wall.
Rupture: if the adventitia can no longer contain the enlarged or damaged wall, a rupture may occur.
Organ and limb problems: narrowing (stenosis) of inflamed vessel areas can reduce blood flow to the brain, arms, legs, or abdominal organs.
These complications explain why careful monitoring and treatment are essential.
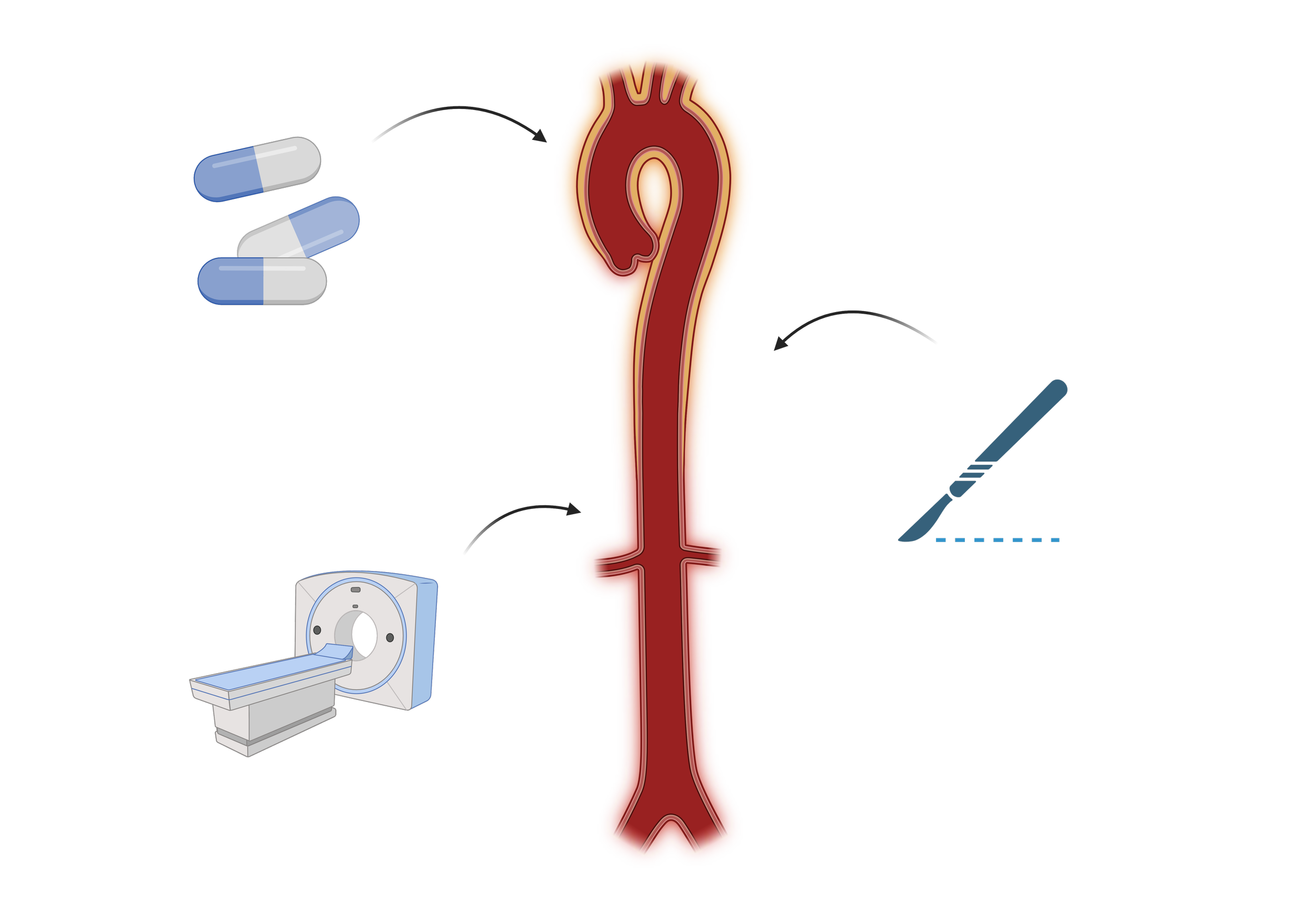
How Is It Treated?
Treatment depends on the cause of inflammation and how much damage has already occurred:
Medication: The first line is usually drugs that reduce inflammation, such as corticosteroids (e.g., prednisone). In autoimmune conditions, stronger immunosuppressive medicines may be needed. If an infection is the cause, antibiotics are given.
Surgery or minimally invasive repair: If the inflammation has caused a large aneurysm or dissection, surgeons may need to repair the damaged aorta with either open surgery (using a graft/prosthesis) or a stent placed inside the vessel.
Ongoing follow-up: Regular imaging (like CT or MRI scans) helps check whether the inflammation is under control and ensures the aortic wall remains stable.
Because inflammatory aortic disease can affect different layers of the wall, from the intima and media to the adventitia, treatment usually requires a combination of medical therapy and, when necessary, surgical repair.